image courtesy IVF@work
This week is UK Fertility Week and today the theme is #FertilityAtWork
I've written about this at length in previous blog posts, which you can check out here:
Nov 18: Fertility At Work
Feb 19: Fertility In The Workplace
Everything I wrote in those posts is (sadly) still just as valid several months on, so please do check them out for more detailed info and insight into the impact of fertility issues in the workplace.
This year I wanted to highlight some new research findings and initiatives that show how this issue is more salient than ever.
Support needs to come at an organisational level
We can only get the support we need from employers if we actually let them know that we're going through fertility issues in the first place.
But if (worst case) we worry that we'll be discriminated against and (best case) that they won't know how to support us - how likely are we to say anything?
New research from LinkedIn found that almost two thirds of workers wouldn’t discuss fertility issues with their employers - but a similar number would be more likely to have a conversation with their employer about fertility if they had training/guidance on how to deal with the conversation.
This fantastic infographic from Dr Uracha Chatrakul Na Ayudhya at Middlesex University highlights the scale of the problem.
Advocating for this change
HR professionals are starting to acknowledge that offering fertility support to employees would make them more competitive in attracting and retaining talent, and that happier employees would be more productive employees.
Which is great. More awareness is good.
But we need more than conversation. We need action.
Much of the coverage in the media about fertility benefits has been around coverage for fertility treatment provided by global corporations. But there's so much more that every company can do - from the small business right up to the multinational.
Claire Ingle is an HR professional and fertility patient who's written about why IVF should be higher on HR's agenda and is speaking out as an activist for change. She is speaking to organisations about the support networks/polices and procedures they have in place (and the most common response is that they simply 'don't') and advocating for change - do check out her IVF@work blog and follow her on Twitter and Instagram
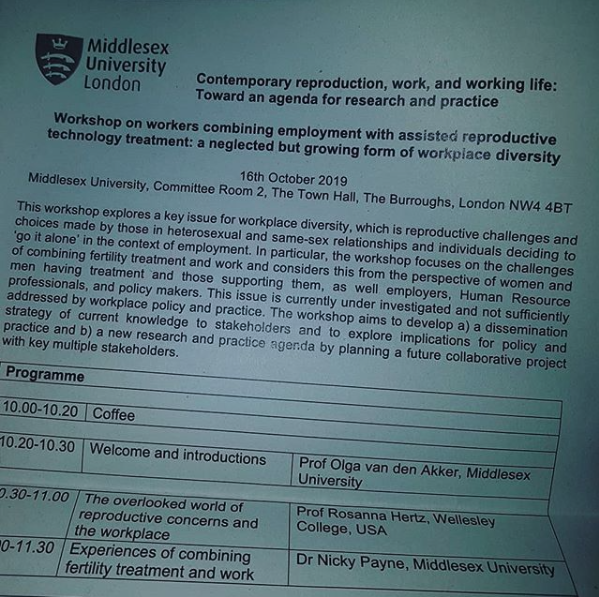
Middlesex University is at the forefront of getting this issue on the agenda, which they described in a recent workshop on 'Contemporary reproduction, work and working life' as 'a neglected but growing form of workplace diversity".
image courtesy IVF@work
Middlesex have collaborated with Fertility Network UK since 2016, leading to the launch of Fertility Network UK's Fertility In the Workplace initiative - offering employers training sessions and policy consultations to help them develop and implement their own fertility policies, as outlined in their Workplace Webinar
Channel 4 recently hit the headlines for their (brilliant) recently launched menopause policy for employees - I hope by this time next year we can see stories about employers launching formal fertility policies in the headlines too...